Help Is Available For Phn
Fortunately,early treatment for shingles can lower your chances of getting PHN.
For some people, the pain becomes refractory, or resistant to treatment, explains Dr. Rosenquist. So we want to treat shingles as fast as we can ideally as soon as somebody feels a tingling or burning sensation, even before a rash develops.
Sheadds that whenever nerve pain is involved, some people respond to treatment andsome dont.
However,medications taken orally or injected that can target the affected nerves may beable to stun the nervous system into behaving properly. That meanstransmitting the appropriate signal to the brain.
Risk Factors For Nerve Pain After Shingles
Researchers have long known that older people are more likely to get PHN, the nerve pain after shingles, but recent studies have found other factors that increase risks.
In one study published in the journal Neurology, researchers — including Dworkin — looked at data from 965 people with shingles. The researchers identified five risk factors for developing PHN in people who had been recently diagnosed with shingles:
- Presence of symptoms before the rash appeared, like numbness, tingling, itching, or pain
- Severe pain during the illness’s initial stages
Importantly, the researchers found the more risk factors you have, the greater the risk of developing PHN.
For instance, 17% of women with shingles and 26% of those who had severe pain went on to get PHN. But 50% of women who were over age 60 and had symptoms before the rash, severe rash, and acute pain went on to get PHN.
New Drug Treatment Reduces Chronic Pain Following Shingles
by Sam Wong05 February 2014
A new drug treatment has been found to be effective against chronic pain in patients who have had shingles.
The researchers hope that the drug might also be effective against other causes of pain caused by nerve damage, known as neuropathic pain, such as diabetes, HIV, nerve injury and cancer chemotherapy, as it targets a mechanism that is not targeted by any existing therapies and has fewer side effects.
Drugs available now have limited success at treating neuropathic pain and often have unpleasant or disabling side effects.
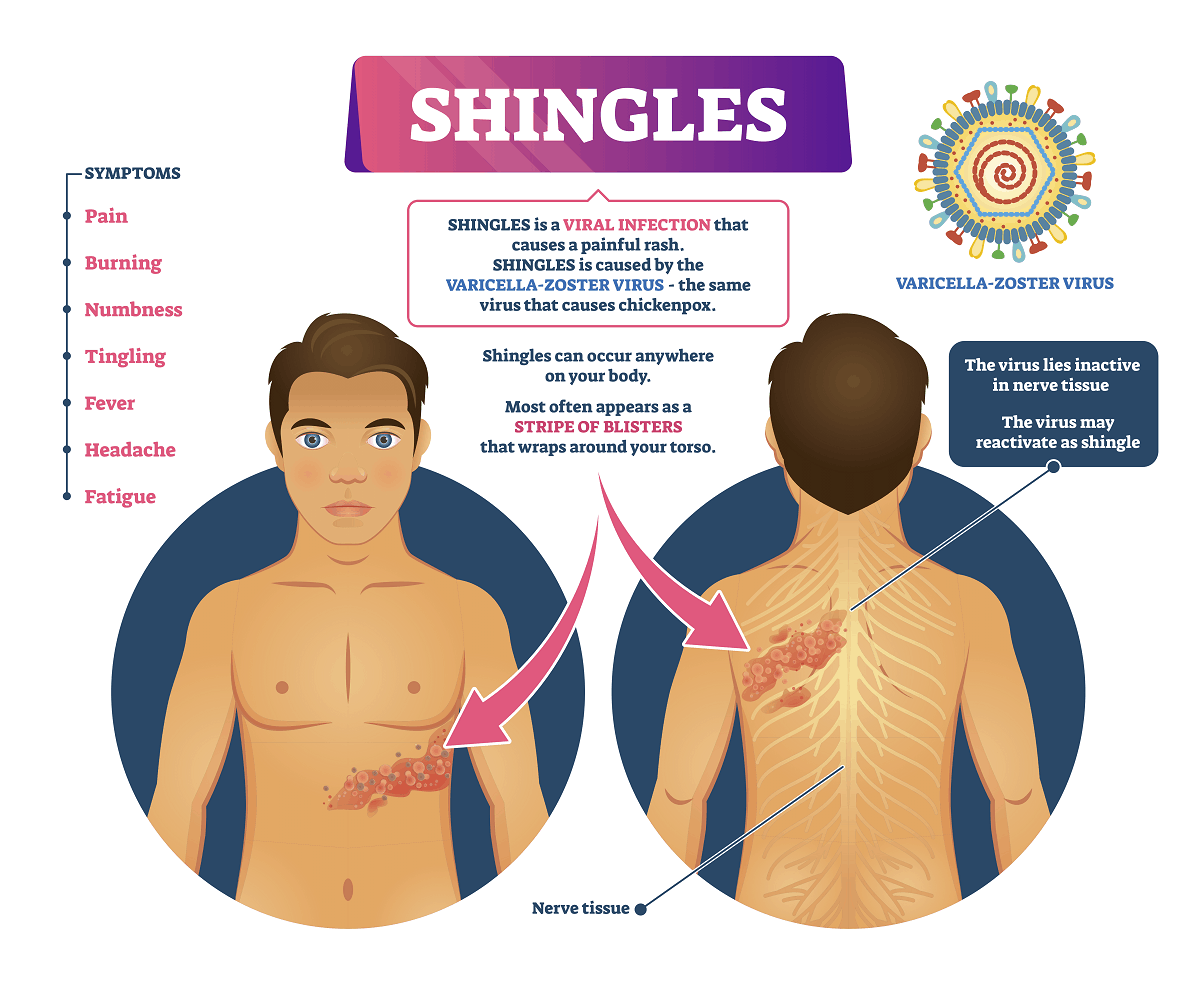
It is estimated that around 190,000 people in the UK get shingles every year, most of them aged over 50. It is caused when a dormant viral infection of a nerve is reactivated, resulting in a painful rash. In most cases, the shingles rash lasts a few weeks, but in some cases the permanent nerve damage caused by the virus results in a chronic neuropathic pain called post-herpetic neuralgia. Around one in 10 people with shingles experiences post-herpetic neuralgia and, once established, it usually causes life-long suffering.
In a study involving 183 patients with post-herpetic neuralgia in six countries, the new drug EMA401 was found to reduce pain and did not cause any serious side effects. The findings are published in The Lancet.
Spinifex Pharmaceuticals, which owns the drug, now plans to conduct a larger trial, possibly testing higher doses of the drug for longer periods of time.
You May Like: What Are The Home Remedies For Shingles
Nerve Blocks For Shingles Pain
The same virus responsible for chicken pox during childhood causes shingles pain as an adult. The virus becomes active in nerve tissue causing severe pain usually on one side of the body. This occurs more frequently in people older than 60, but can occur in younger individuals. Shingles usually presents in sharp pain followed by a rash. The more likely areas to be affected include the chest or abdomen, and less frequently, the face, the arms, or the legs.
Reasons for treatment
A shingles infection causes a very severe nerve inflammation that if left untreated can evolve into a more severe form of the disease called post-herpetic neuralgia. This disease is a complication of shingles where nerves and their blood supply have been severely damaged from inflammation. Typically. the older you are and the more pain you have during your shingles episode, the more likely it is for you to develop permanent pain. Blocking the pain in the affected nerves using strong numbing medicines and anti-inflammatories will shorten the actual shingles pain and may decrease the chance of developing severe nerve damage and chronic pain.
Procedures
Spinal Cord Or Peripheral Nerve Stimulation
These are often used to treat several different types of neuropathic pain. Electrodes are placed underneath the skin along the affected peripheral nerves. Before using this technique, doctors will do a test using a wire electrode to get a sense of how the patient will respond.
After the electrodes have been placed above the peripheral nerve, a weak electrical current is sent to the nerve. By stimulating a sensory pathway that doesnt cause pain, experts believe that this electrical signal to the brain can trick the brain into turning off the painful signal, bringing relief to the patient.
You May Like: Can You Get Shingles On Your Breast
Understanding Chronic Shingles Pain
If you had chickenpox as a child, you may be at risk of developing shingles as an adult, as both conditions are produced by the same virus: varicella-zoster. Even after the condition has improved and symptoms have disappeared, people never truly recover from the disease. The virus lies dormant in the body and has the potential to resurface later in life. Research suggests that the virus comes back as an individual gets older and their immune system becomes weaker. The pain management specialists at Southwest Spine and Pain Center are able to help patients understand what shingles pain is and how to prevent it from becoming chronic.
Understanding Shingles Pain
Shingles typically begins with pain and other symptoms such as sensitivity to touch, numbness, or tingling. After a few days, the condition progresses into a painful, blistering rash. Shingles patients may also experience fevers, headaches, and body aches. Depending on the location of the pain, patients may mistake their symptoms with heart, lung, or kidney problems. Nevertheless, some people with shingles never develop a rash, or really intense, sharp pains. Some shingles patients have reported pain flare-ups from certain triggers like brushing skin across furniture or from the wind hitting their bodies.
Prevention
Avoiding Chronic Pain
If You Have Shingles Symptoms Get Treatment Now And You May Avoid Permanent Nerve Pain
Shingles, a viral infection of the nerve roots, affects 1 million people in the U.S each year. Most people recover from their bout, but for as many as 50% of those over age 60 who have not been treated, the pain doesn’t go away. It can last for months, years, or even the rest of their lives.
These people have what’s called postherpetic neuralgia , the result of the shingles virus damaging the nerves of the skin. In some cases, the pain is mild. In others, even the slightest touch — from clothing or even a breeze — can be excruciating.
“PHN causes a great deal of suffering and high social costs,” says Robert H. Dworkin, PhD, a professor in the department of anesthesiology at the University of Rochester Medical Center in Rochester, N.Y. “It can severely disrupt people’s lives.”
But the good news is that there are drugs that can help treat and even prevent PHN, and doctors are learning more about who is at greatest risk of developing this debilitating condition.
Don’t Miss: What To Do If You Have Shingles
A Word About The Shingles Vaccine
If you are age 60 or over and have not had shingles, talk to your doctor about getting the shingles vaccine. Not only will it reduce your risk of developing shingles, but if you do develop shingles, youll be more likely to have a mild case. And, just as important, youll be much less likely to develop PHN if youve had the vaccine.
Shingles And Your Eyes
If the shingles rash breaks out on the face, near the eye, the vision may be affected. An ophthalmologist should be consulted right away when pain or other symptoms of shingles affect the eye or the area near the eye.
Shingles painand other symptoms from an outbreak of herpes zosterusually lasts between three to five weeks. Most people experience shingles once, but in some instances, people will continue to experience pain. When this happens, its called postherpetic neuralgia .
Don’t Miss: Can You Lay Shingles On Wet Tar Paper
What You Can Do About Nerve Pain That Lingers After Shingles
Chronic pain that continues after a case of shingles is called postherpetic neuralgia . It is estimated that about 20% of patients will experience this type of nerve pain as a complication of shingles.
Those who have had chickenpox are at risk of developing shingles later in life. People who develop PHN are generally age 60 and older. Although there is no cure for PHN, there are several methods of pain management that can ease symptoms. Fortunately, the type of pain that arises from postherpetic neuralgia improves over time.
Neuralgia affects the nerves, causing structural and functional damage. It can feel like a stabbing or burning pain that radiates along the affected nerve.
Neuropathic pain is not caused by an external injury or stimuli but originates from inside the nervous system. When the herpes-varicella zoster virus is reactivated in the form of shingles, scar tissue forms alongside nerves, creating pressure, and sending pain signals to the brain.
How Common Is Postherpetic Neuralgia
Varicella-zoster virus causes both chickenpox and shingles. About 99% of Americans over age 40 have had chickenpox. About one in three people in the U.S. develop shingles in their lifetime. Some 10 to 18% of people who get shingles will develop postherpetic neuralgia. Postherpetic neuralgia is the most common complication of shingles.
You May Like: Shingles Rash Pictures On Back
The Best Pain Doctor For Shingles Pain Treatment Is Roziermd
If you have shingles pain, you should immediately seek the care and treatment of a reputable pain doctor.
Dr. Antonio Rozier is a highly experienced and reputable pain management doctor. He is the best pain doctor for shingles pain treatment in Dallas, Mansfield & TX. He is equipped with different interventional techniques and treatments for various types of pain including shingles pain.
If you have shingles pain or you are searching for a doctor that is very experienced in the treatment of shingles pain, Dr. Rozier is highly recommended.
What Are Typical Symptoms Of Post

The symptoms of PHN are very often limited or localised to the area of skin where the shingles outbreak first occurred.1 This is why PHN is often referred to as being a type of localised neuropathic pain.3
The chronic pain associated with PHN can be described as burning pain, stabbing pain, itching or aching. Patients with PHN often have hypersensitive skin, like a bad sunburn, and may feel severe pain from the touch of clothing on the affected area, a condition doctors call allodynia.1,4
Don’t Miss: Does Stress Bring On Shingles
When To See A Doctor
Chronic intercostal neuralgia can greatly impact a persons quality of life.
The condition can be extremely uncomfortable. Chronic pain from intercostal neuralgia can also lead to reduced movement and poor sleep quality. It can also make it difficult for a person to breathe.
Also, intercostal neuralgia has some symptoms in common with other potentially serious health conditions. These include:
For this reason, it is important for anyone with prolonged or acute intercostal neuralgia to see a doctor immediately.
People should also see a doctor if they experience other symptoms of shingles.
What Is Shingles And Postherpetic Neuralgia
Shingles is caused by the varicella-zoster virus, the virus that also causes chickenpox. In a person who has been exposed to chickenpox — or its vaccine — the virus never really goes away. It can lie dormant in the body’s nerves.
In most cases, it stays that way. But in some — especially people with immune systems weakened by disease or treatment — the virus can reappear. This is likely to happen years or decades after the person had chickenpox.
When it comes back, the virus can cause shingles, a rash that often appears as a band on one side of the body. Early shingles symptoms can include:
- Flu-like symptoms
Itching, tingling, or extreme pain where the rash is developing may come next, and the pain can be moderate to severe.
Are you contagious? Though people who haven’t had chickenpox can catch that condition from you, the shingles itself isn’t contagious.
For reasons that experts don’t really understand, the pain of shingles lingers for some. If the pain lasts for at least 3 months after the shingles rash has healed, a person is diagnosed with PHN. In some people, the pain will subside. In others, it won’t.
“We don’t have any idea why the pain goes away in some people and not others,” says Dworkin. But the longer you have PHN — especially after a year — the less likely it is to resolve, he says.
Read Also: What Is Shingles And Is It Contagious
Best Treatments For Lasting Shingles Pain
Postherpetic Neuralgia Pain: What Works, What Doesn’t
Doctors call it postherpetic neuralgia or PHN. It’s caused by nerve damage left behind by a case of shingles. Shingles itself comes from reactivation of a chickenpox virus, varicella zoster. The virus travels down nerve fibers to cause a painful skin rash.
When the rash goes away, the pain usually goes with it. But for 12% to 15% of people the pain remains. If your shingles pain lasts eight to 12 weeks after the rash goes away, you’re part of an “unfortunate minority,” says pain researcher Andrew S.C. Rice, MD, of Imperial College, London.
“Among people with PHN, some have their pain resolve in the first year to 18 months after the shingles rash goes away,” Rice tells WebMD. “But if they have pain longer than that, it is not going to go away on its own. In either case, a person must deal with the pain.”
How Is Postherpetic Neuralgia Treated
If shingles is caught within the first three days of its outbreak, your healthcare provider may prescribe the antiviral medication acyclovir , valacyclovir or famciclovir . These medications help the rash/blisters heal faster, keep new sores from forming, decrease pain and itching and reduce length of pain after sores have healed.
If your shingles outbreak is not caught early, your healthcare providers has many options to manage your postherpetic neuralgia symptoms.
If your pain is mild, your healthcare provider may recommend:
- Acetaminophen or NSAIDs such as ibuprofen .
- Creams and patches include lidocaine and capsaicin .
If your pain is more severe, your healthcare may prescribe:
- Antiseizure drugs gabapentin and pregabalin .
- Antidepressants, such as escitalopram , quetiapine or amitriptyline.
- Botulinum toxin injections in the area where you are having pain.
Theres no clear-cut superior treatment for PHN. Your provider may need to try more than one medication or prescribe the use of several medications at the same time. You and your provider will discuss options and what makes sense to try for you. Contact your provider if your pain is not lessening after taking your medicine. Take all your medications exactly as prescribed.
Also Check: What Are The Best Architectural Shingles
How Can This Pain Be Managed
If your doctor is able to identify an underlying cause for the neuropathic pain, treating it may reduce and even eliminate the pain.
For example, diabetes is a common cause of neuropathic pain. Proper diabetes care which includes a healthy diet and regular exercise may eliminate or reduce neuropathic pain.
Taking care of blood sugar levels can also prevent worsening pain and numbness.
Treatment Of Herpes Zoster
The treatment of herpes zoster has three major objectives: treatment of the acute viral infection, treatment of the acute pain associated with herpes zoster and prevention of postherpetic neuralgia. Antiviral agents, oral corticosteroids and adjunctive individualized pain-management modalities are used to achieve these objectives.
Also Check: What Type Of Shingles Are Best
Shingles And Nerve Paths
Shingles is caused by a reactivation of the virus that causes chickenpox. Only people whove had chickenpox or chickenpox vaccines can develop shingles. Having a chickenpox vaccine can lead to shingles because the vaccine contains the virus that causes chickenpox.
Shingles isnt contagious, but people who have not had chickenpox can develop chickenpox if they come in contact with open blisters of somebody with shingles.
After your body fights off a chickenpox infection, the herpes zoster virus remains dormant in your cranial nerves and spinal ganglia until it becomes reactivated. Spinal ganglia are nerve cells that connect your spinal cord to nerves in your body and limbs.
The virus reactivates when your immune system is no longer able to suppress it. Reactivation most commonly occurs in older adults because the immune system tends to get weaker with age, as well as in people with suppressed immune systems.
Once the virus is active, it usually spreads down sensory nerve fibers that lead from your spinal cord to your skin. These nerves carry sensory information like feelings of pain, itchiness, or pressure from your skin to your spinal cord and brain.
Once the virus gets to the end of these sensory nerves, it reaches your skin and usually leads to a rash. This rash often shows up in one or two nearby areas of skin called dermatomes.
A dermatome is an area of your skin where the sensation is supplied by one spinal nerve.
The Emotional Toll Of Nerve Pain After Shingles
Researchers are not just looking at biological and neurological risk factors for PHN. Dworkin was also a co-author of a study looking at psychological risk factors, too. The results were published in the Journal of Pain in 2005.
“It certainly looks like psychological stress can be a potent risk factor for PHN,” Dworkin tells WebMD.
The study showed that people with shingles who went on to develop PHN were more likely to have had symptoms of personality disorders, hypochondria, intense worry about their disease, and other bodily complaints.
Dworkin says previous studies have already shown a connection between stress and shingles development.
“One study even found that the risk of developing PHN was higher in people who were living alone when they developed shingles than people living with others,” Dworkin says, perhaps indicating that social isolation increases the risks of PHN.
Recommended Reading: How To Relieve Symptoms Of Shingles