Shingles Vaccine May Be Safe For Ra Patients Treated With Biologics
Although the shingles vaccine is still not recommended for people taking certain types of drugs for rheumatoid arthritis , a study suggests that the vaccine does not increase short-term risk of shingles in these patients, and may decrease longer-term risk. These results were published in the Journal of the American Medical Association.
Rheumatoid arthritis affects an estimated 1.3 million adults in theUnited States. The condition causes pain, swelling, and stiffness of joints, and can lead to permanent joint damage.
Treatment of RA often begins with methotrexate or another disease-modifying antirheumatic drug . If this initial treatment does not adequately control the RA, patients may move on to treatment with a newer, biologic DMARD such as a TNF inhibitor. Although these drugs provide effective RA treatment for many people, they also suppress parts of the immune system and can increase the risk of infection.
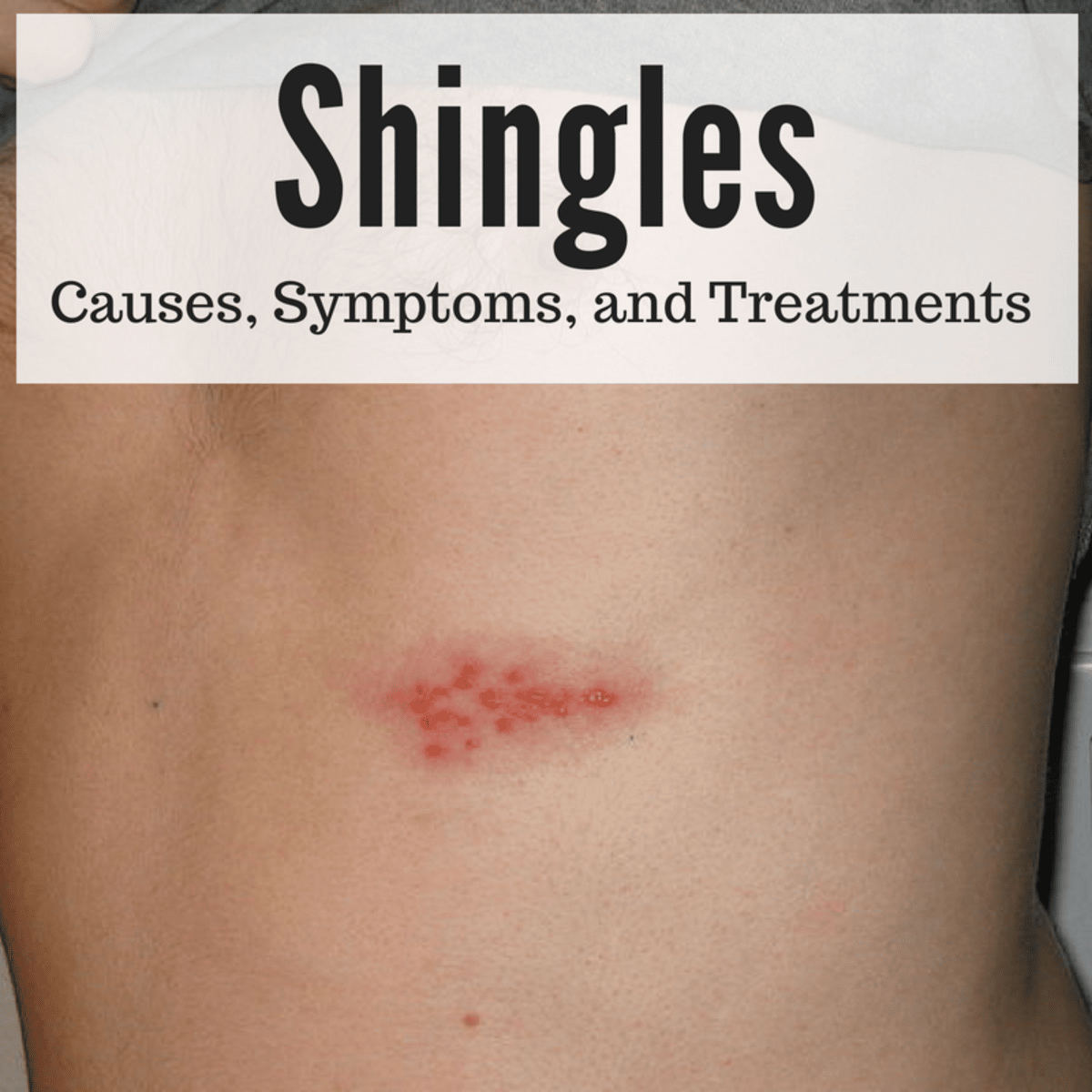
Shingles results from reactivation of the chickenpox virus. Shingles causes a painful rash that usually develops in a single stripe on one side of the body or face. The condition can affect anyone whos had chickenpox, but is most common in older people or those with a weakened immune system. People with immune-mediated conditions such as RA are also at increased risk of shingles.
References:
What Causes A Shingles Outbreak
Shingles, also called herpes zoster, is a painful condition that most often affects adults over 50. While in most cases, it is not a serious condition, it can be extremely unpleasant.
So, what causes shingles and how do you get it?
Have you considered clinical trials for Shingles?
We make it easy for you to participate in a clinical trial for Shingles, and get access to the latest treatments not yet widely available – and be a part of finding a cure.
Shingles Vaccine Ok For People With Immune Disorders
Herpes zoster vaccine may get another look in patients being treated for autoimmune diseases such as rheumatoid arthritis.
New research from the University of Alabama at Birmingham casts doubt on the long-standing belief that the vaccine for shingles should not be given to patients taking biologics for auto-immune diseases such as rheumatoid arthritis. The findings were published today in the Journal of the American Medical Association.
Shingles, or herpes zoster, is a reactivation in adults of the varicella virus that causes chicken pox in children. The U.S. Food and Drug Administration recommends a vaccine for shingles for people older than 60, but not for individuals taking anti-tumor necrosis factor therapies or other biologics commonly used to treat immune-mediated diseases.
The vaccine is a live attenuated vaccine, and the long-standing opinion in the medical community is that patients with certain immune-related diseases receiving immunosuppressive therapies like biologics are at increased risk of contracting varicella from the vaccine itself, said Jeffrey Curtis, M.D., lead author of the study and associate professor in the division of Clinical Immunology and Rheumatology in UABs School of Medicine. However, that opinion has not been definitively bolstered by scientific studies.
The study was funded by the Agency for Healthcare Research and Quality and the National Institutes of Health.
Also Check: Shingles Shots How Far Apart
Shingles Vaccine Reduces Your Risk Of Getting Shingles
While there is no cure for shingles, getting the shingles vaccine can greatly reduce your risk of getting this disease.
Shingles vaccine reduces risk
The CDC recommends the shingles vaccine for healthy adults who are 50 years of age or older.
If you think you may already have shingles, treatment is important. It can reduce your pain and how long the rash lasts.
Find out how dermatologists diagnose and treat this condition at, Shingles: Diagnosis and treatment.
3 Centers for Disease Control and Prevention . Prevent Shingles: Get vaccinated. Page last reviewed July 23, 2018. Last accessed March 28, 2019.
ImageGetty Images
ReferencesCenters for Disease Control and Prevention . Prevent Shingles: Get vaccinated. Page last reviewed July 23, 2018. Last accessed March 28, 2019.
Dooling KL, Guo A, et al. Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines. Morb Mortal Wkly Rep 2018 67:103-8.
Can Children Get Shingles
It’s rare, but children can get shingles. Typically, pediatric shingles happen in children who were exposed to chickenpox very young. This includes in-utero exposure if the child’s mother had chickenpox 5 to 21 days before giving birth.
These children have a small chance of developing shingles before the age of 5 because their immune system is not yet fully developed.
Older children exposed to chickenpox in kindergarten or younger can rarely get shingles a few years later or in adolescence, but this is unusual. The chickenpox vaccine has significantly reduced the incidence.
Recommended Reading: How Long Does The Nerve Pain Last From Shingles
Recurrent Shingles: Herpes Zoster Can Strike More Than Once
Heres what to know about recurrent shingles and risk factors.
Individuals who have experienced the painful and often debilitating condition known as shingles would like to think that its a 1-and-done infection. Unfortunately, although a reoccurrence of shingles is not common, it can and does happen due to the innate nature of the varicella zoster virus that causes the latent infection.
VZV does not discriminate by age. The virus is at the root of both the childhood infection known as chickenpox and the adult infection shingles. Both chickenpox and shingles are characterized by a blistering red rash. Other shared symptoms include fever, fatigue, and headache.
Once the primary infection resolves, VZV moves into the dorsal root ganglia where it remains dormant for decades. It can then reactivate as HZ and possibly cause serious complications like postherpetic neuralgia and postherpetic itch .
According to the CDC, an estimated 1 million cases of HZ occur annually in the United States. Although the incidence rate in the general population is about 4 cases per 1000 individuals, it increases to about 1 case per 100 individuals among people who are 60 years and older.1
Other risk factors include age , gender , high anxiety and stress levels, certain immunosuppressive therapies, cancer, autoimmune diseases like HIV/AIDS and lupus, and chronic diseases like diabetes, hypertension, and chronic obstructive pulmonary disease.1
References
How Is Shingles Diagnosed
Your healthcare provider will do a complete physical exam and ask about your medical history, specifically about whether you have ever had chickenpox.
Your healthcare provider will likely know right away that it is shingles based on the unique rash. The rash usually appears one area on one side of the body or face. It appears as red spots, small fluid- or pus-filled vesicles, or scabs.
The healthcare provider may also take skin scrapings for testing.
Read Also: How Do You Know If You Got Shingles
Risk Increased By 50% In The First Month
SAN FRANCISCO — Patients with an autoimmune disease, such as rheumatoid arthritis , have a significantly elevated risk for having a stroke within a month of developing herpes zoster, researchers reported here.
After adjustment for multiple potential confounders, the incidence rate ratio for autoimmune disease patients being hospitalized with an ischemic stroke within 30 days after developing herpes zoster reactivation was 1.50 compared with their rate in subsequent years 2 to 6, according to Leonard H. Calabrese, DO, of the Cleveland Clinic, and colleagues.
Action Points
- Note that this study was published as an abstract and presented at a conference. These data and conclusions should be considered to be preliminary until published in a peer-reviewed journal.
The risk of stroke remained high throughout the first year after the shingles episode, with an incidence rate ratio of 1.30 compared with their risk in year 2, he reported in a plenary session at the at the American College of Rheumatology annual meeting.
“These data are important as we now live in an era of increasing concern over herpes zoster,” Calabrese said.
Zoster is associated with significant morbidity even in its less serious forms, and stroke is one of its potential complications.
However, little is known about the risk among patients with autoimmune diseases — who have an elevated risk for both zoster and stroke.
He urged clinicians to advocate for zoster vaccination.
Disclosures
Autoimmune Disease + Shingles = 50% Increase In Stroke Risk
People who have autoimmune diseases, including psoriasis, who get incident herpes zoster have a 50 percent increased stroke risk within a month of developing shingles, according to a new study.
People who have autoimmune diseases, including psoriasis, who get incident herpes zoster have a 50 percent increased stroke risk within a month of developing shingles, according to a new study.
Read: Herpes is everywhere
The frequency of herpes zoster, an opportunistic infection caused by varicella zoster virus, is increasing among patients on immunosuppressive therapies, including biologics.
Researchers from the Cleveland Clinic in Ohio, analyzed Medicare data from 2006 to 2012 to identify nearly 51,000 patients with incident herpes zoster and diagnoses of one of these autoimmune diseases: ankylosing spondylitis, inflammatory bowel disease, psoriasis, psoriatic arthritis or rheumatoid arthritis. They followed patients for ischemic stroke hospitalizations after shingles diagnoses, comparing one-, six- and 12-month follow ups.
Read: Antiviral vaccine rebounds versus herpes
The study highlights the need to develop strategies to reduce herpes zoster risk among immunosuppressed patients, according to the authors.
Study author according to Leonard H. Calabrese, D.O., vice chair of rheumatic and immunologic diseases at the Cleveland Clinic, told Dermatology Times the results suggest two things to dermatologists.
Also Check: How Often Do You Get A Shingles Shot
Stroke Risk Doubles In Autoimmune Disease And Shingles Patients
Patient with autoimmune diseases, like psoriasis, and infected with herpes zoster â commonly known as shingles â have a 50% higher risk of suffering a stroke.
Patients with autoimmune diseases, like psoriasis, and infected with herpes zoster commonly known as shingles have a 50% higher risk of suffering a stroke.
Its interesting to note the incidence of shingles has increased over the years, especially for patients treated with immunosuppressive therapies and biologics.
Leonard H. Calabrese, DO, vice chair of rheumatic and immunologic diseases, Cleveland Clinic, and team analyzed Medicare data from 2006 to 2012 to distinguish approximately 51,000 patients with shingles as well as any autoimmune disease like: ankylosing spondylitis, inflammatory bowel disease , psoriasis, psoriatic arthritis, or rheumatoid arthritis.
The researchers monitored the patients particularly for ischemic stroke hospitalizations following their shingles diagnoses for one, six, and 12-month follow-ups.
After the six-month mark, results indicated the incidence rate of hospitalized ischemic stroke was 9.8 for each 1,000 patient years, compared with a rate of 8.7 for 1,000 in two to six years.
Also, for two-thirds of the more complicated shingles patients, the hazard ratio for stroke was 3.2 in the first 30 days, compared to 1.6 in the uncomplicated group.
Risk Of Shingles In Ra Patients
Rheumatoid arthritis significantly increases the risk of shingles and related complications. Studies suggest that people with RA have a 1.5 to 2 times higher risk of developing shingles than the general population.
When people with RA do get shingles, they are also more likely to develop serious medical complications. For example, a 2017 study found that people with RA who contracted shingles were twice as likely to have a stroke in the following months.
Its not entirely clear why people with RA are more likely to get shingles. Some people with RA have a weakened immune system, which increases the chance of developing a variety of illnesses and infections. RA flare-ups also increase the bodys overall level of inflammation, which has been linked to both shingles and PHN.
Additionally, many people with RA take immunosuppressantsdrugs that work to reduce the bodys natural immune responseto treat their symptoms and prevent flare-ups. Several common rheumatoid arthritis medications have been found to increase the risk of shingles, including:
Don’t Miss: Google Show Me What Shingles Look Like
Are Vaccines Effective Against Shingles
Being vaccinated against chickenpox lowers your risk of shingles. While the vaccine can cause shingles, it is at a much lower rate.
There is also an approved vaccine, Shingrix. This vaccine is delivered in two doses and is recommended at the age of 50 and to adults with weakened immune systems. It is also recommended that people vaccinated with the older vaccine, Zostavax, get Shingrix as it is substantially more effective.
In older adults, Shingrix is more than 90% effective. Shingrix is a reactogenic vaccine, meaning it tends to have more side effects than some other vaccines. However, the side effects are much less severe than getting shingles. Consider scheduling your vaccine for a time when you can take a day off work in case you get side effects.
How Are Shingles Diagnosed

Shingles are typically diagnosed by examining the rash. The shingles rash is similar to that experienced during chickenpox but is typically more localized.
Testing for antibodies to the varicella virus is not typically done to diagnose shingles, as most people carry it, and those antibodies are found in people who have been vaccinated. But in most cases, the shingles rash is distinctive enough to provide a solid diagnosis.
Don’t Miss: Lowes Hip And Ridge Shingles
Age And Weak Immune System Increase Your Risk Of Getting Shingles
Although anyone who has had chickenpox can get shingles, your risk of developing shingles increases with age. Most people get shingles in their 50s or later in life.
Its rare to get shingles before 40 years of age. Scientists are still studying why this happens. Its likely that your immune system keeps the virus dormant. When the immune system starts to weaken, which may start in your 50s, the virus can wake up.
Age increases your risk of getting shingles
Many people who had chickenpox dont remember having it and are unaware that they can get shingles.
Anyone who has a weakened immune system also has an increased risk of getting shingles. This includes people who have:
-
Some cancers, such as leukemia or lymphoma
-
Human immunodeficiency virus
-
To take medication that suppresses the immune system, such as people living with an organ transplant, severe psoriasis, or advanced psoriatic arthritis
-
To receive certain cancer treatments, such as chemotherapy
Where The Fda And Cdc Stand
According to the CDC, people ages 50 and up and immunocompromised adults ages 19 and older should get two doses of Shingrix to prevent shingles, PHN, and other possible complications. Shingrix is effective and safe for most people, including people with autoimmune disorders.
The CDC currently recommends that people with chronic medical conditions, such as RA, get the shingles vaccine. Additional CDC guidelines for people with autoimmune conditions are as follows:
- Shingrix is usually delivered in two doses, two to six months apart. If you are immunocompromised, your healthcare provider may suggest that you get your second Shingrix dose after just one to two months instead.
- Its usually best to wait until your symptoms are well-controlled to get Shingrix. If youre currently having a severe RA flare-up, you should typically wait until you feel better to get the shingles vaccine.
- If youre taking immunosuppressants to manage RA symptoms, talk to your healthcare provider about the vaccine schedule that works best for you.
The Food and Drug Administration approved the use of Shingrix in 2017 for people ages 50 and older. In 2019, the FDA approved Shingrix for immunocompromised adults ages 18 and older. The FDA hasnt yet issued any specific guidelines about Shingrix and RA.
Recommended Reading: How Does A Person Get Shingles Rash
What Everyone Should Know About The Shingles Vaccine
Shingles vaccination is the only way to protect against shingles and postherpetic neuralgia , the most common complication from shingles.
CDC recommends that adults 50 years and older get two doses of the shingles vaccine called Shingrix to prevent shingles and the complications from the disease. Adults 19 years and older who have weakened immune systems because of disease or therapy should also get two doses of Shingrix, as they have a higher risk of getting shingles and related complications.
Your doctor or pharmacist can give you Shingrix as a shot in your upper arm.
Shingrix provides strong protection against shingles and PHN. In adults 50 years and older who have healthy immune systems, Shingrix is more than 90% effective at preventing shingles and PHN. Immunity stays strong for at least the first 7 years after vaccination. In adults with weakened immune systems, studies show that Shingrix is 68%-91% effective in preventing shingles, depending on the condition that affects the immune system.
What Are The Possible Side Effects Of Shingrix
Studies show that Shingrix is safe. The vaccine helps your body create a strong defense against shingles. As a result, you are likely to have temporary side effects from getting the shots. The side effects might affect your ability to do normal daily activities for 2 to 3 days.
Most people got a sore arm with mild or moderate pain after getting Shingrix, and some also had redness and swelling where they got the shot. Some people felt tired, had muscle pain, a headache, shivering, fever, stomach pain, or nausea. Some people who got Shingrix experienced side effects that prevented them from doing regular activities. Symptoms went away on their own in about 2 to 3 days. Side effects were more common in younger people.
You might have a reaction to the first or second dose of Shingrix, or both doses. If you experience side effects, you may choose to take over-the-counter pain medicine such as ibuprofen or acetaminophen.
Guillain-Barré syndrome , a serious nervous system disorder, has been reported very rarely after Shingrix. There is also a very small increased risk of GBS after having shingles.
If you experience side effects from Shingrix, you should report them to the Vaccine Adverse Event Reporting System . Your doctor might file this report, or you can do it yourself through the VAERS websiteexternal icon, or by calling 1-800-822-7967.
If you have any questions about side effects from Shingrix, talk with your doctor.
Don’t Miss: How Many Doses Of The Shingles Vaccine Are Needed