Rebooting The Nervous System
Its like restarting a computer, Dr. Rosenquist says. When its running slowly or acting weird, you restart it. We are trying to turn that nerve off. When it comes back on, hopefully, it will send an appropriate transmission as opposed to a pain transmission.
Treatmentoptions for PHN patients include:
Patientswith refractory PHN rarely need opioid pain medication. However,you should be evaluated by a physician. We cant make a blanket statement abouttreatment. It is individualized, she says.
What Is Shingles And Postherpetic Neuralgia
Shingles is caused by the varicella-zoster virus, the virus that also causes chickenpox. In a person who has been exposed to chickenpox — or its vaccine — the virus never really goes away. It can lie dormant in the body’s nerves.
In most cases, it stays that way. But in some — especially people with immune systems weakened by disease or treatment — the virus can reappear. This is likely to happen years or decades after the person had chickenpox.
When it comes back, the virus can cause shingles, a rash that often appears as a band on one side of the body. Early shingles symptoms can include:
- Flu-like symptoms
Itching, tingling, or extreme pain where the rash is developing may come next, and the pain can be moderate to severe.
Are you contagious? Though people who haven’t had chickenpox can catch that condition from you, the shingles itself isn’t contagious.
For reasons that experts don’t really understand, the pain of shingles lingers for some. If the pain lasts for at least 3 months after the shingles rash has healed, a person is diagnosed with PHN. In some people, the pain will subside. In others, it won’t.
“We don’t have any idea why the pain goes away in some people and not others,” says Dworkin. But the longer you have PHN — especially after a year — the less likely it is to resolve, he says.
Have Shingles Get Treatment Take Action
If you have shingles, it’s important to talk to your doctor about your risk for developing PHN. Ask whether preventative treatment with antiviral drugs makes sense. If your doctor says it’s not necessary, ask why.
The full implications of the psychological risk factors for PHN aren’t clear yet, says Dworkin. But he suggests that people with shingles should try to stay active and connected.
“If psychological distress is a risk factor for PHN,” he says, “then we think that people who have shingles might benefit from getting out and not being isolated and homebound.”
You might make an effort to stay connected to family and friends and not to dwell on your symptoms. Also, keep in mind that even if you do develop PHN, there are treatments that can help.
“We have about a half dozen types of drugs that are used as first-line treatments for PHN,” says Dworkin. They include lidocaine patch , pregabalin , gabapentin , capsaicin , carbamazepine , tricyclic antidepressants, and painkillers.
The most important thing is to get prompt medical attention if you think you might have shingles.
“If you have a one-sided rash — especially if you’re over 50 — see your doctor right away,” says Dworkin. “It could be shingles. And we know that prompt treatment can dramatically reduce the likelihood of developing long-term pain.”
Show Sources
Don’t Miss: How To Schedule Shingles Vaccine At Cvs
Hearing Loss And Facial Weakness
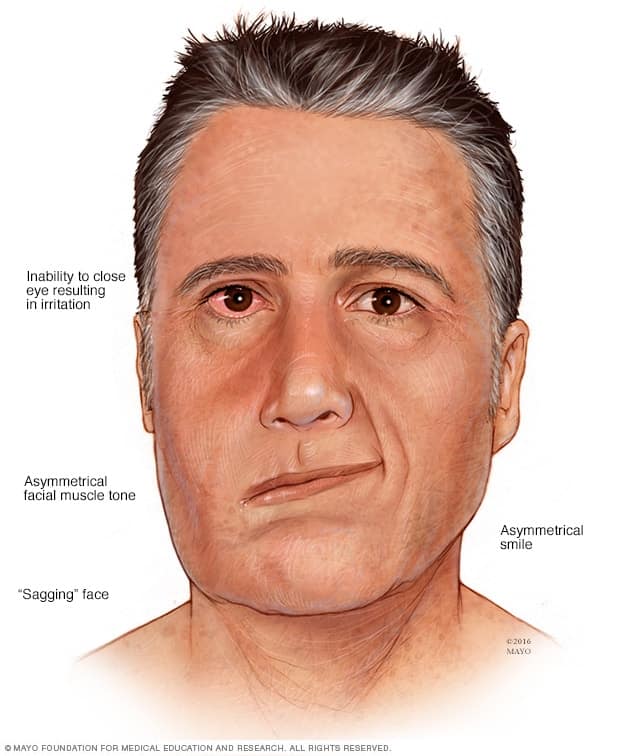
Complications of herpes zoster oticus and Ramsay Hunt syndrome might include hearing loss and facial weakness. For most people, these are temporary symptoms, but it is possible for the damage to become permanent, especially if shingles is left untreated.
Ramsay Hunt syndrome accounts for up to 12% of facial paralysis. In some cases, it has a worse outcome than Bells palsya condition that causes temporary weakness in the muscles of the face.
What Is Ramsay Hunt Syndrome
Ramsay Hunt syndrome is a complication of varicella-zoster virus infections, including chickenpox or shingles . Other names for the condition include herpes zoster oticus and Ramsay Hunt syndrome type 2. It got its name when an American army officer and neurologist named James Ramsay Hunt first described the disorder in 1907.
If you had chickenpox as a child, the virus that caused it can remain inactive in your nerves for years. Shingles occurs when the previously dormant varicella-zoster virus reactivates. The reactivation of the varicella-zoster virus in your facial nerve is called Ramsay Hunt syndrome.
Ramsay Hunt syndrome causes facial nerve paralysis and intense ear pain. In addition, it may cause a painful rash on your ear, face or mouth.
Read Also: Red Light Therapy For Shingles
How Rare Is Ramsay Hunt Syndrome
Ramsay Hunt syndrome affects about 5 out of every 100,000 people each year in the U.S.
However, some researchers think the condition is sometimes undiagnosed or misdiagnosed. This makes its true frequency more difficult to determine.
The disorder is the second most common cause of facial nerve paralysis, accounting for about 7% of all cases. Bells palsy is the most common cause of facial nerve paralysis.
Are There Other Ways To Ease The Pain
Most people with postherpetic neuralgia use medication to control their symptoms. But there are other ways to control the pain, too. They include:
TENS : You use a device that shoots tiny electrical currents into the area of pain on the skin. This helps block the pain.
Cold packs: Try a gel-filled one to numb the area unless cooler objects make your neuralgia worse.
Comfortable clothes: Go for looser fits and fabrics such as cotton and silk.
Don’t Miss: Side Effects Of Second Shingles
The Emotional Toll Of Nerve Pain After Shingles
Researchers are not just looking at biological and neurological risk factors for PHN. Dworkin was also a co-author of a study looking at psychological risk factors, too. The results were published in the Journal of Pain in 2005.
“It certainly looks like psychological stress can be a potent risk factor for PHN,” Dworkin tells WebMD.
The study showed that people with shingles who went on to develop PHN were more likely to have had symptoms of personality disorders, hypochondria, intense worry about their disease, and other bodily complaints.
Dworkin says previous studies have already shown a connection between stress and shingles development.
“One study even found that the risk of developing PHN was higher in people who were living alone when they developed shingles than people living with others,” Dworkin says, perhaps indicating that social isolation increases the risks of PHN.
What Are The Symptoms Of Postherpetic Neuralgia
Common postherpetic neuralgia symptoms include:
- Burning, sharp, jagging or aching pain in the area where the shingles rash appeared.
- Itchiness or numbness at or near the area of the former rash.
- Pain that is constant or comes and goes. Pain typically lasts, on average, for three months after the rash has healed, but can last for more than a year or longer.
- Pain at affected skin area can be brought on even with a light touch .
- Pain gets worse at night or in heat or cold temperatures.
Don’t Miss: What Does Shingles Look Like At Start
How Can You Prevent Spreading The Virus
You cant give shingles to someone else, but the varicella-zoster virus is very contagious. If you have shingles and you expose someone else who has not had chickenpox or the chickenpox vaccine, you can give them the virus. Theyll get chickenpox, not shingles, but this puts them at risk for shingles later on.
Youre contagious when your blisters are oozing, or after they break and before they crust over. Do the following to avoid spreading the virus to others:
- Keep your rash covered, especially when the blisters are active.
- Try not to touch, rub, or scratch your rash.
- Wash your hands thoroughly and often.
Avoid contact with people whove never had chickenpox or the chickenpox vaccine, especially:
Shingles On The Face: Complications And Treatment
Potential for serious complications is very real.
The red rash and lesions associated with shingles can erupt anywhere on the human body. It all depends on which nerves are affected by the reactivation of the varicella zoster virus that remained in the body after an earlier case of chickenpox.
Although the front and back of the torso are the usual sites of the rash, the face will be affected when the virus reactivates in the trigeminal nerve, which handles face and motor functions. When this happens, the patient is at risk for potentially serious complications like facial pain, numbness, tingling, or paralysis damage to the eyes, and hair loss.
The shingles rash generally appears on just 1 side of the affected body part, and the face is no exception. The fluid-filled blisters can extend to cover the mouth, eye, ear, forehead, nose, and scalp. Early diagnosis and treatment can help limit the length of the infection and its complications, including postherpetic neuralgia.
Two of the most serious threats from shingles on the face are herpes zoster ophthalmicus and herpes zoster oticus, which involves the ear.
Herpes zoster ophthalmicus , or ocular shingles, is a growing health risk in the United States, according to an article published in the American Academy of Ophthalmologys EyeNet Magazine.1 It reports that cases are on the rise and account for approximately 10% of all shingles cases.1
Reference
Read Also: What Is The Disease Called Shingles
Why Is Shingles Bad
Shingles is not fun for anyone, but its negative impact can be significantly worse for some.
The General Experience: Herpes zoster causes a distressing rash that typically occurs in a stripe around the left or right side of the body. This will last for weeks with pain, tingling and itchiness. Medical News Today describes the pain as being a constant dull, burning, or gnawing pain, or sharp, stabbing pain that comes and goes.
In rare cases the rash may not be limited to a single stripe and will instead appear more like a widespread chickenpox rash.
Other symptoms can include fever, headache, chills and an upset stomach.
While having one episode of the shingles rash is common, multiple episodes can happen over time in some cases.
Lasting Nerve Damage:WebMD reports that up to 50 percent of those over age 60 who havent been treated for their shingles will develop postherpetic neuralgia . The CDC states that approximately 10 to 13 percent of people who get shingles will experience PHN. PHN occurs when the varicella-zoster virus damages the nerves.
Those with postherpetic neuralgia experience mild to devastating pain when touched. The pain can be very mild or be devastating depending on the specific case. PHN can cause issues for patients for a few months, years or even for the rest of their lives.
Shingles And Postherpetic Neuralgia

After you have had chickenpox, the virus lies inactive in nerve tissue near your spinal cord and brain. Years later, the virus may reactivate as shingles. Postherpetic neuralgia is the most common complication of shingles. PHN is pain resulting from a herpes zoster outbreak along the trigeminal nerve. Postherpetic neuralgia occurs if your nerve fibers are damaged during an outbreak of shingles.
Damaged fibers cannot send messages from your skin to your brain as they normally do. Instead, the messages become confused and exaggerated, causing chronic pain. The most common area to have PHN is along the torso, but pain in the face can also occur. The sensation may be of intense burning or stabbing, and it may feel as if it is shooting along the course of the affected nerve.
PHN typically starts during the shingles outbreak, but lasts after the rash and blisters have healed. Chicken pox causes shingles later in life. People over the age of 60 have an increased risk of shingles. Treatment for PHN does not cure it, but aims to minimize its symptoms.
Also Check: What To Put On Shingles For Itch
How To Treat Facial Nerve Paralysis
The treatments of facial nerve paralysis vary widely because the right therapy depends on the cause. This is one of the reasons that diagnosis of the underlying condition is so important.
Treatments include:
- Steroids may help speed the natural recovery of Bells palsy.
- Antibiotics are required for the treatment of bacterial meningitis.
- Surgery may be necessary to repair a nerve thats injured or to remove a tumor.
- Drainage of an infected abscess or facial infection may be needed.
- Blood thinners and other stroke-directed treatments may help treat a stroke.
- Migraine medication can treat an ongoing migraine.
Treatment must be specific to the cause because any therapy for facial nerve paralysis will not be helpful unless it targets the underlying problem.
In addition to these specific interventions, physical therapy can speed recovery from facial nerve paralysis of any cause.
Sometimes recovery is complete, but often there is only partial recovery after facial nerve paralysis. Muscles can begin to atrophy when they arent used. Rehabilitation can help you rebuild your facial muscle strength after facial nerve paralysis.
Types Of Facial Nerve Paralysis
Facial nerve paralysis is often described as central or peripheral. Central facial nerve paralysis is caused by a problem affecting the brain. It causes weakness in the lower part of the face. Peripheral facial nerve paralysis is caused by a problem affecting the nerve. It causes weakness in the whole face, including the forehead.
You May Like: Where Are Tamko Shingles Made
Multidermatomal Varicella Zoster With Multiple Cranial Nerve Involvement Presenting With Partial Ophthalmoplegia In An Immunocompetent Woman
ABSTRACT: Varicella-zoster virus is rarely the cause of multiple cranial nerve palsies. Partial or complete ophthalmoplegia can occur with VZV infection, but the optimal treatment for this condition is unknown. We report the case of a 79-year-old immunocompetent woman who presented with multidermatomal VZV, herpes zoster ophthalmicus, multiple cranial nerve palsies, and partial unilateral ophthalmoplegia. Our report highlights the use of corticosteroids and antivirals to treat her VZV-associated partial ophthalmoplegia.
The case of an immunocompetent patient who presented with partial ophthalmoplegia, a rare complication of varicella-zoster virus infection, suggests that corticosteroids can be used in conjunction with antiviral medication to treat the condition in select patients.
Key points
- Varicella zoster can affect both sensory and motor cranial nerves, and is a rare cause of complete or partial ophthalmoplegia in both immunocompromised and immunocompetent patients.
- The underlying mechanism of cranial nerve involvement is unknown but may involve direct viral infection and postinfectious inflammation of the cranial nerves.
- There is little evidence to guide treatment of varicella-zoster virus ophthalmoplegia, but the use of corticosteroids in addition to antivirals may target inflammation involved in the pathogenesis of this condition.
The Dialectic Of Pain: Synthesizing Acceptance And Change
Dr. Deborah Barrett offers a framework and tools to help people improve their quality of life, just as they are, while also reducing pain and suffering. Her work draws from empirically based cognitive and behavioral interventions, and she practices what she preaches every day.
Facial pain can be described in many wordsbut if you had to choose just one, what would it be? The YPC recently shared how we would describe TN in one word and how we plan to overcome TN.
Dr. Julie Pilitsis, Chair of the Department of Neuroscience & Experimental Therapeutics Professor of Neurosurgery Neuroscience and Experimental Therapeutics, Albany Medical Center and FPA Medical Advisory Board member presents an overview of trigeminal neuralgia and other neuropathic facial pains.
Two members of the facial pain community, Ally Kubik and Jodi Irwin, share their experiences of being mothers while coping with facial pain.
Dr. Julie Pilitsis discusses ways to get your pain to manageable levels.
Jeffrey A. Brown, MD, FACS, FAANS First, some basic requirements: there are a lot, but that is the point, too. Doctors educated in the United States are granted their MD
Read Also: Can You Get Shingles Without A Rash
How Is Ramsay Hunt Syndrome Treated
Ramsay Hunt syndrome treatment may include various medications. Your healthcare provider may prescribe:
- An antiviral medication to treat the infection or decrease symptoms, such as acyclovir or valacyclovir.
- A corticosteroid to reduce inflammation of the nerve, such as prednisone.
- A pain reliever to reduce pain.
- A variety of possible medications to relieve symptoms of vertigo.
- An anti-seizure medicine, such as carbamazepine, to treat persistent pain .
Natural treatment for Ramsay Hunt syndrome includes using a cold compress to reduce your pain. You may also consider wearing an eye patch. If youre unable to close your eye, you risk damaging your cornea due to irritation. You may also want to use artificial tears or eye lubricants to prevent your eye from drying out.
If you have complete facial paralysis, your healthcare provider may perform a surgical procedure. The surgery can help relieve the pressure on your facial nerves.
Controversies In The Care Of Facial Pain
Dr. Raymond Sekula, Professor of Neurosurgery at the University of Pittsburgh School of Medicine and Director of the Cranial Nerve Disorders Program at UPMC, and FPA Medical Advisory Board member reviews the challenges that can complicate the care of people with neuropathic facial pain.
Dr. Michael Lim gives an overview of trigeminal neuralgia.
Dr. Gary Stanton explains how acupuncture can help manage TN pain.
For many people with facial pain, weather can cause pain flares. Learn why weather can affect your facial pain and what you can do to minimize it.
Neuropathic pain is a chronic pain condition, and refers to all pain initiated or caused by a lesion or dysfunction in the nervous system.
Medical disorders that affect the facial nerve may be the cause of your pain. Learn more about underlying conditions that cause face pain.
Dr. Jeffrey Brown, Chairman of the Facial Pain Associations Medical Advisory Board, interviews Dr. Hossein Ansari on medical causes of neuropathic facial pain.
Dr. Raymond F. Sekula, Jr. explains the microvascular decompression procedure, a treatment option for trigeminal neuralgia.
Dr. Michael Lim discusses the pros and cons of the various surgical options for treating TN.
Neuromodulation can relieve various types of facial pain. Learn more about neuromodulation and whether it can help your face pain.
Facial pain can create fears and doubts. Learn about taking control of your life with facial pain.
Read Also: Pictures Of Shingles Without Blisters